When the freshly graduated medical Doctor Ignaz Semmelweis started a position at the Vienna General Hospital in 1846, he was looking forward to kick-start his career at the most renowned institution of its kind. 8,000 patients were admitted to the hospital each year, and no other clinic enjoyed a higher reputation for the teaching of obstetrics. The hospital was a beacon of modern medicine and its maternal clinics aimed to revolutionize the treatment of becoming mothers and newly born infants.
Unsolved deaths and ignorant elites
Once he took up his position, Semmelweis found out that despite the hospital’s stellar reputation, reality on the ground looked starkly different. One in six mothers died within a week after giving birth, the highest death rate of any clinic in Europe. The hospital was, as Semmelweis put it, “truly an institution of death.”
It was decades before the germ theory of disease was discovered by Pasteur and John Lister, and the Hospital’s management assumed that poor air quality was the cause of the problem. This was addressed through improved ventilation and the burning of medicinal herbs, common procedures at the time. You will not be shocked to hear they did not yield any measurable results.
Semmelweis was as just as clueless, but, unlike his superiors, he didn’t pretend otherwise. Instead, he tried to systematically understand what was happening and in in doing so, set out to invent methods that would later revolutionize medicine. He took an ample interest in statistics and experimental design, which was at the time unusual for a medical doctor, and he spent much of his time collecting and analyzing data.
Using data to uncover the truth
Previously, Semmelweis had noticed that the first of the two maternal clinics had a terrible reputation outside of the hospital. Becoming mothers were begging on their knees not to be admitted, and when he started to compare mortality rates between the two clinics, he was able to confirm that the chance of dying in the first clinic was three times higher than in the second one. After isolating every possible cause – including differences in diet, the way the laundry was done or even religious practices – the only systematic difference he could make out was that the first clinic was used to train medical students, while the second one was mainly used to train midwives.
This observation again raised eyebrows with some of Semmelweis’ superiors. Did he imply that midwives did a better job of handling patients than academically trained future doctors? The superiority of modern science was not to be questioned, and the implicit, uncodifiable skills midwives had been passing on over generations were little understood or appreciated among academic elites.
Semmelweis’s ultimate breakthrough however was triggered by a tragic event. His friend Jakob Kolletschka accidentally poked his finger with a scalpel while instructing medical students during an autopsy. He died shortly after, and his own autopsy revealed similarities with the women that had been dying of childbed fever. Semmelweis developed the hypothesis that the medical students performing postmortem examinations in the morning infected women in the maternal clinic in the afternoons.
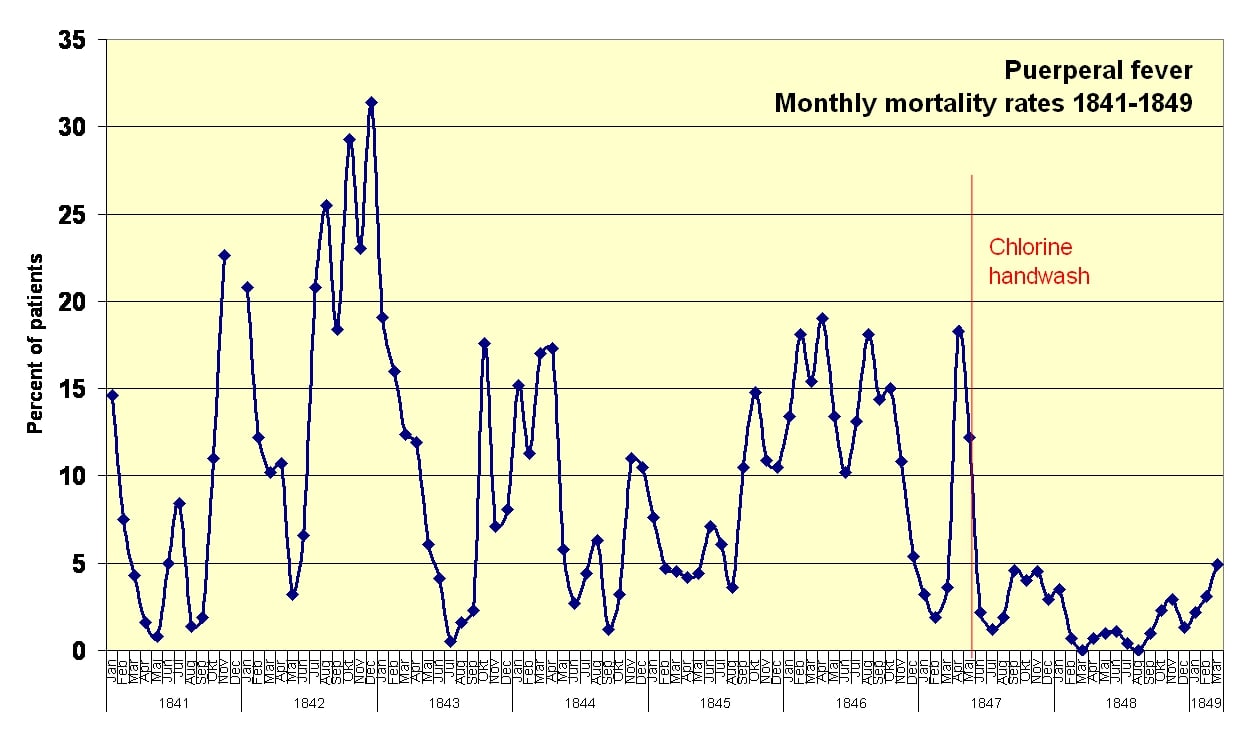
Semmelweis himself had noticed an irritating smell on his hands after autopsies and got rid of it by cleaning them with chlorinated solution. As a consequence, he put up bowls with chlorinated lime (which was cheaper than pure chlorinated solution) in the maternal clinics and asked his colleagues to sanitize their hands before seeing patients. The impact of this was astonishing: two months later death rates fell from 18% to under 2% and close to zero in the following year.
The short-term risks and long-term rewards of speaking truth to power
As a result, you would think that Semmelweis was hailed by his peers and went on to spread the word about his discovery across the continent.
Well, you would be wrong.
Semmelweis was disciplined by his bosses, who believed that his discovery was way too simplistic. A single cause could not possibly be responsible for this much suffering and death, especially not one as banal and easy-to-fix.
Semmelweis was pushed out, the hand sanitizer tossed out and the hospital went back to smoking out evil spirits with incense and dried sage. In all likelihood, this drove up deaths again, but no one kept track anymore. Semmelweis returned to his home country Hungary to practice medicine and go on a crusade against the shortcomings of modern medicine. 10 years after leaving Vienna, he published the findings he had been collecting over the years, which were groundbreaking to say the least. Years later, Pasteur and Robert Koch (who had quarrels of their own) would uncover the foundations of microbiology, thereby explaining why Semmelweis’s findings were accurate and giving them further credence.
Unfortunately, Semmelweis would not live to witness the fame and respect he gained through his work. He became increasingly quirky over the years and picked fights with various renowned figures from the medical community. He ended up in a mental institution where he died of an antiseptic shock. Conspiracy theories are connected to his passing until this day, and the circumstances of his death do seem dodgy. Among other things, his final autopsy was conducted by his former superior from Vienna.
While Semmelweis’s story is tragic, his findings lived on to change medicine and save millions of lives. He became known as “The Savior of Mothers” and is still revered around the world. At least in part, his systematic analyses also laid the foundations of randomized control trials (RCT), which are today considered the gold standard of assessing the effects of medical treatments.
Three takeaways from the Semmelweis story
While I don’t want to equate his doing with our work in the modern business world, his story holds many truths that we can apply to leadership, analytics and personal philosophy:
1. Intuition and data analysis must go hand in hand
Simple hunches can go a long way if you test them systematically. Semmelweis knew nothing about microorganisms, yet he was able to prove that hand sanitation could bring down the mortality rate at the hospital by more than 90%. Takeaway: Follow your intuition but make sure to collect data and systematically. It is the only way to know if you are headed in the right direction.
2. People might not like what you tell them, and that’s ok
Dreaming of rock-star level fame and popularity? At least in the short-term, don’t work with data. In fact, collecting data and drawing the right conclusions from it can make you more enemies than friends. This is especially true if a) you are challenging status quo and b) if you operate in a domain that was previously not data-driven. But don’t worry: history looks favorably on those who speak truth to power.
3. Don’t separate science from practice
Despite having data, never tell year-long practitioners what to do without trying to understand their craft. In the mid-19th century, much of the modern medical community looked down on midwives, a profession that had been built and whose practices had been passed on and refined over centuries, and who actually did a much better job of delivering newborns in the mid-19th centuries than academically educated doctors. To make a comparison with the world of business: If you want to use a mathematical model to tell your sales or marketing teams what to do, better make sure in advance that you speak their language and acknowledge the intangibles that make up their craft. Otherwise, you will not only fall on deaf ears, but miss important insights that can enrich your understanding of reality.
BACK TO ALL ARTICLES